The human shoulder, a marvel of biomechanical engineering, offers an unparalleled range of motion, enabling a vast array of daily activities from reaching overhead to intricate hand movements. This incredible mobility, however, comes at a cost: a susceptibility to injury and inflammation. Among the most common culprits of shoulder pain and dysfunction is shoulder tendonitis, a condition characterized by inflammation or irritation of the tendons surrounding the shoulder joint. This comprehensive exploration delves into the intricacies of shoulder tendonitis, covering its anatomy, causes, symptoms, diagnosis, treatment options, and crucial aspects of rehabilitation and prevention.
Table of Contents
ToggleAnatomy of the Shoulder and its Tendons
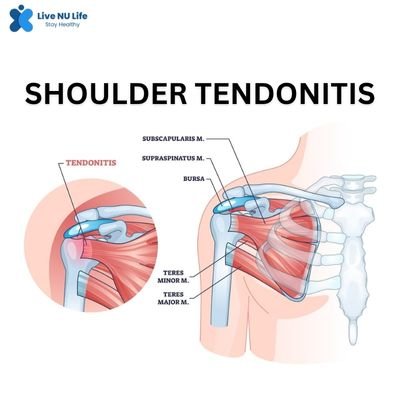
To truly grasp shoulder tendonitis, an understanding of the shoulder’s complex anatomy is paramount. The shoulder joint is a ball-and-socket joint formed by three main bones: the humerus (upper arm bone), the scapula (shoulder blade), and the clavicle (collarbone). This articulation allows for movement in multiple planes, making it the most mobile joint in the body.
Crucial to the shoulder’s stability and movement are its surrounding soft tissues, particularly the tendons. Tendons are strong, fibrous cords of connective tissue that connect muscles to bones. In the shoulder, several key tendons are often implicated in tendonitis:
- Rotator Cuff Tendons: This group of four muscles and their tendons are the primary stabilizers and movers of the shoulder. They form a “cuff” around the head of the humerus. The four rotator cuff muscles are:
- Supraspinatus: Located at the top of the shoulder blade, its tendon passes through a narrow space beneath the acromion (a bony projection of the scapula). It is primarily responsible for initiating arm abduction (lifting the arm away from the body). The supraspinatus tendon is the most commonly affected in rotator cuff tendonitis due to its vulnerable position.
- Infraspinatus: Located on the back of the shoulder blade, it helps with external rotation (rotating the arm outward).
- Teres Minor: A smaller muscle also on the back of the shoulder blade, it assists with external rotation.
- Subscapularis: Located on the front of the shoulder blade, it aids in internal rotation (rotating the arm inward).
- Inflammation of any of these tendons leads to rotator cuff tendonitis, which is the most prevalent form of shoulder tendonitis.
- Biceps Tendon: The biceps muscle, located on the front of the upper arm, has two heads (long and short). The long head of the biceps tendon runs through a groove in the humerus and attaches to the top of the shoulder socket. While primarily known for elbow flexion, its role in the shoulder involves stabilizing the humeral head. Biceps tendonitis, often occurring in conjunction with rotator cuff issues, causes pain in the front of the shoulder.
- Other Tendons: While less common, other tendons around the shoulder, such as those of the deltoid muscle (which gives the shoulder its rounded contour), can also experience inflammation, though this is less frequently diagnosed as primary tendonitis.
Pathophysiology: What Happens in Tendonitis?
Tendonitis essentially means “inflammation of a tendon.” This inflammation can range from microscopic tears and swelling to significant degeneration of the collagen fibers that make up the tendon. The body’s inflammatory response, while intended to heal, can paradoxically cause pain and further damage if persistent.
Over time, chronic tendonitis can lead to a condition called tendinosis. Unlike tendonitis, which is primarily inflammatory, tendinosis involves a degeneration of the tendon’s collagen without significant inflammation. This distinction is crucial for treatment, as anti-inflammatory medications are less effective for tendinosis, which requires strategies focused on stimulating collagen repair and remodeling. Often, the terms are used interchangeably, but from a medical perspective, understanding the underlying pathology can guide more targeted interventions.
Causes of Shoulder Tendonitis
Shoulder tendonitis typically arises from a combination of factors, often categorized as either acute (sudden onset) or chronic (gradual onset).
- Overuse and Repetitive Activities: This is by far the most common cause. Any activity that involves repetitive overhead movements can strain the shoulder tendons. This includes:
- Sports: Throwing sports (baseball, javelin), swimming, tennis, volleyball, weightlifting (especially overhead presses).
- Occupations: Painters, carpenters, electricians, mechanics, hairdressers, and anyone whose job requires frequent arm elevation or sustained awkward positions.
- Hobbies: Gardening, cleaning, reaching for objects on high shelves.
- Poor Posture: Slouching or rounded shoulders can alter the biomechanics of the shoulder joint, narrowing the space beneath the acromion (subacromial space) where the rotator cuff tendons pass. This “impingement” can lead to friction and inflammation of the tendons.
- Age-Related Degeneration: As we age, tendons naturally become less elastic and more susceptible to wear and tear. Blood supply to tendons also diminishes, making them slower to heal. This is why shoulder tendonitis is more common in middle-aged and older adults.
- Acute Injury: A sudden, forceful movement or direct impact to the shoulder can sometimes lead to acute tendonitis or even a partial tendon tear, which then becomes inflamed.
- Underlying Medical Conditions: Certain systemic conditions can increase the risk of tendonitis:
- Diabetes: Affects collagen synthesis and blood flow, making tendons more vulnerable.
- Thyroid Disorders: Can contribute to musculoskeletal problems.
- Rheumatoid Arthritis and other inflammatory arthropathies: Can cause widespread inflammation, including in tendons.
- Improper Technique: In sports or occupational tasks, incorrect form can place undue stress on the shoulder tendons, leading to injury.
- Muscle Imbalances: Weakness in certain shoulder muscles (e.g., rotator cuff) or tightness in others (e.g., pectoralis muscles) can disrupt the normal movement patterns of the shoulder, putting excessive strain on the tendons.
Symptoms of Shoulder Tendonitis
The symptoms of shoulder tendonitis can vary in intensity and presentation, but commonly include:
- Pain:
- Location: Typically localized to the front, side, or back of the shoulder, often radiating down the upper arm, sometimes to the elbow.
- Character: Aching, throbbing, dull, or sharp pain.
- Aggravating Factors: Worsens with overhead activities, lifting, reaching, or sleeping on the affected side. Pain is often most noticeable at night, disrupting sleep.
- Relieving Factors: Rest and ice may provide temporary relief.
- Tenderness: The affected tendon will be tender to the touch, especially when palpated over the area of inflammation.
- Stiffness: The shoulder may feel stiff, especially after periods of inactivity or in the morning.
- Weakness: A feeling of weakness when attempting to lift or move the arm, particularly against resistance. This can be due to pain inhibition or actual tendon damage.
- Crepitus or Clicking: A grinding, crackling, or clicking sensation may be felt or heard with shoulder movement, indicating friction or inflammation.
- Limited Range of Motion: Difficulty or pain with certain movements, especially overhead reaching, external rotation, or internal rotation.
Diagnosis of Shoulder Tendonitis
Diagnosing shoulder tendonitis typically involves a combination of medical history, physical examination, and imaging studies.
- Medical History: The doctor will inquire about the onset of pain, aggravating and relieving factors, types of activities performed, any previous injuries, and relevant medical conditions.
- Physical Examination: This is a crucial step. The doctor will:
- Observe Posture: Look for any asymmetries or postural abnormalities.
- Palpate: Gently press on various areas of the shoulder to identify tenderness, particularly over the rotator cuff tendons and biceps tendon.
- Assess Range of Motion: Actively and passively move the arm in various directions to identify limitations and pain patterns.
- Perform Special Tests: Conduct specific tests that put stress on individual tendons (e.g., Neer’s impingement test, Hawkins-Kennedy test for rotator cuff impingement; Speed’s test, Yergason’s test for biceps tendonitis). These tests help pinpoint the affected tendon and differentiate tendonitis from other shoulder conditions.
- Assess Strength: Test the strength of various shoulder muscle groups.
- Imaging Studies:
- X-rays: While X-rays do not show soft tissues like tendons, they are useful for ruling out other conditions that can cause shoulder pain, such as fractures, arthritis (bone spurs can contribute to impingement), or calcific tendonitis (calcium deposits in the tendon).
- Ultrasound: This non-invasive imaging technique is excellent for visualizing soft tissues in real-time. It can effectively show tendon inflammation, swelling, and sometimes partial tears. It’s often used for its accessibility and ability to dynamic assessment.
- MRI (Magnetic Resonance Imaging): MRI provides detailed images of soft tissues, including tendons, muscles, ligaments, and cartilage. It is considered the gold standard for diagnosing tendon tears (partial or full-thickness), severe inflammation, and other subtle soft tissue abnormalities that might be missed by X-rays or ultrasound.
Treatment of Shoulder Tendonitis
The treatment for shoulder tendonitis is typically conservative and aims to reduce pain, inflammation, and restore function. The approach depends on the severity of the condition and the specific tendon involved.
- Conservative Management (First-Line Treatment):
- Rest and Activity Modification: This is paramount. Avoid activities that aggravate the pain, especially overhead movements. This doesn’t necessarily mean complete immobilization, but rather modifying or temporarily ceasing offending activities. Relative rest allows the inflamed tendon to heal.
- Ice Application: Apply ice packs to the affected area for 15-20 minutes, several times a day, especially after activity or when pain is acute. Ice helps reduce inflammation and pain.
- Pain Relief and Anti-Inflammatory Medications:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Over-the-counter NSAIDs like ibuprofen (Advil, Motrin) or naproxen (Aleve) can help reduce pain and inflammation. Stronger prescription NSAIDs may be used in some cases.
- Topical Pain Relievers: Gels or creams containing NSAIDs can be applied directly to the skin over the painful area.
- Physical Therapy: This is a cornerstone of recovery and is crucial for long-term success. A physical therapist will design a personalized program that includes:
- Modalities: Therapeutic ultrasound, electrical stimulation (TENS), or cold laser therapy may be used to reduce pain and inflammation.
- Range of Motion Exercises: Gentle exercises to restore full shoulder mobility without aggravating pain.
- Strengthening Exercises: Progressive strengthening of the rotator cuff muscles, scapular stabilizers, and deltoid to improve shoulder stability and function. This is critical for preventing recurrence.
- Stretching: Addressing any muscle tightness around the shoulder and chest.
- Posture Correction: Education on proper posture and ergonomic adjustments to reduce stress on the shoulder.
- Activity Modification and Ergonomics: Guidance on how to perform daily tasks and sports activities in a way that minimizes stress on the shoulder.
- Corticosteroid Injections: If conservative measures are insufficient, a corticosteroid injection (cortisone shot) directly into the subacromial space (for rotator cuff tendonitis) or around the biceps tendon can provide significant, but temporary, pain relief and reduce inflammation. These injections are not a cure and should be used judiciously due to potential side effects like tendon weakening or damage with repeated injections. They are typically used to create a “window of opportunity” for physical therapy to be more effective.
- Platelet-Rich Plasma (PRP) Therapy: This involves injecting a concentrated solution of a patient’s own platelets (rich in growth factors) into the injured tendon. The aim is to stimulate healing and tissue regeneration. While promising, more research is needed to solidify its efficacy for all types of tendonitis.
- Advanced or Surgical Management (Less Common):
Surgery is rarely needed for isolated shoulder tendonitis. It is typically reserved for cases where:
- Conservative treatment has failed after 6-12 months.
- There is a significant structural issue contributing to the tendonitis, such as a large bone spur causing persistent impingement.
- There is a significant tear in the tendon (e.g., full-thickness rotator cuff tear) that is unlikely to heal with conservative measures and is causing significant functional limitation.
Surgical procedures may include:
- Arthroscopic Debridement: Cleaning out inflamed tissue and smoothing rough edges of bone that may be impinging on the tendon.
- Acromioplasty (Subacromial Decompression): Reshaping the acromion bone to create more space for the rotator cuff tendons, relieving impingement. This is often done arthroscopically (minimally invasive).
- Tendon Repair: If there is a significant tear, the surgeon may repair the torn tendon back to the bone.
Recovery and Rehabilitation
The recovery process from shoulder tendonitis varies depending on the severity of the condition, the individual’s adherence to treatment, and their overall health.
- Acute Phase (Pain and Inflammation Control): Focus on rest, ice, pain medication, and gentle range of motion exercises as tolerated.
- Subacute Phase (Restoring Mobility and Initial Strengthening): Gradual introduction of strengthening exercises, focusing on rotator cuff and scapular stabilization. Continued emphasis on proper mechanics.
- Chronic Phase (Advanced Strengthening and Return to Activity): Progressive increase in resistance and complexity of exercises. Sport-specific or occupation-specific drills to prepare for return to full activity. Emphasis on proper technique and warm-up.
Key aspects of rehabilitation:
- Consistency: Adhering to the physical therapy program consistently is crucial.
- Patience: Tendons heal slowly. Rushing the process can lead to re-injury.
- Progressive Loading: Gradually increasing the stress on the tendon is essential for strengthening and remodeling.
- Listen to Your Body: Pain is a signal. Respect it and modify activities as needed.
- Warm-up and Cool-down: Always warm up before activity and cool down afterward.
Prevention of Shoulder Tendonitis
Preventing shoulder tendonitis is often more effective than treating it. Key preventive strategies include:
- Proper Technique: Learn and use correct form for sports, exercises, and occupational tasks. Consider professional coaching or ergonomic assessments.
- Gradual Progression: When starting new activities or increasing intensity, do so gradually to allow your body to adapt. Avoid sudden spikes in activity.
- Regular Stretching and Strengthening: Incorporate exercises that strengthen the rotator cuff and scapular stabilizers, and stretches that maintain shoulder flexibility.
- Maintain Good Posture: Be mindful of your posture throughout the day, especially when sitting or working at a computer. Avoid slouching.
- Ergonomic Workstation Setup: Adjust your desk, chair, and computer monitor to promote good posture and reduce shoulder strain.
- Adequate Rest and Recovery: Allow sufficient time for your muscles and tendons to recover between workouts or demanding activities.
- Listen to Your Body: Pay attention to early signs of pain or discomfort and address them promptly. Don’t push through pain.
- Cross-Training: Engage in a variety of activities to avoid repetitive stress on the same muscle groups.
- Warm-up and Cool-down: Always perform a proper warm-up before any physical activity and a cool-down afterward.
Want to dive deeper into health and fitness? Click here to explore more on how to live a healthier, fitter life.
Conclusion
Shoulder tendonitis, while a common and often debilitating condition, is highly treatable. By understanding the anatomy of the shoulder, the causes of tendonitis, and adhering to a well-structured treatment and rehabilitation plan, individuals can significantly reduce pain, restore function, and prevent recurrence. The emphasis on conservative management, particularly physical therapy, alongside activity modification and preventive measures, empowers individuals to regain control over their shoulder health and enjoy a pain-free, active lifestyle. Remember, early diagnosis and intervention are key to a successful outcome, so if you experience persistent shoulder pain, consulting a healthcare professional is the first and most important step.
Also interested in learning about autoimmune diseases? Click here to read our blog on how to prevent autoimmune disease.
Know more about Shoulder Tendonitis. Click here….